Urine formation involves millions of nephrons, as you may not be aware. Yes, what appears to be a simple task is actually a complex process essential to our body’s survival. Let’s learn more about the processes involved in the production of urine.
The liquid waste output of the human body is urine. It includes waste materials produced by numerous bodily metabolic processes, such as urea, uric acid, salts, water, and others. The kidneys, which are the main excretory organs, are where it develops. The nephrons are the kidneys’ basic anatomical and operational unit. Urine production requires the participation of millions of nephrons.
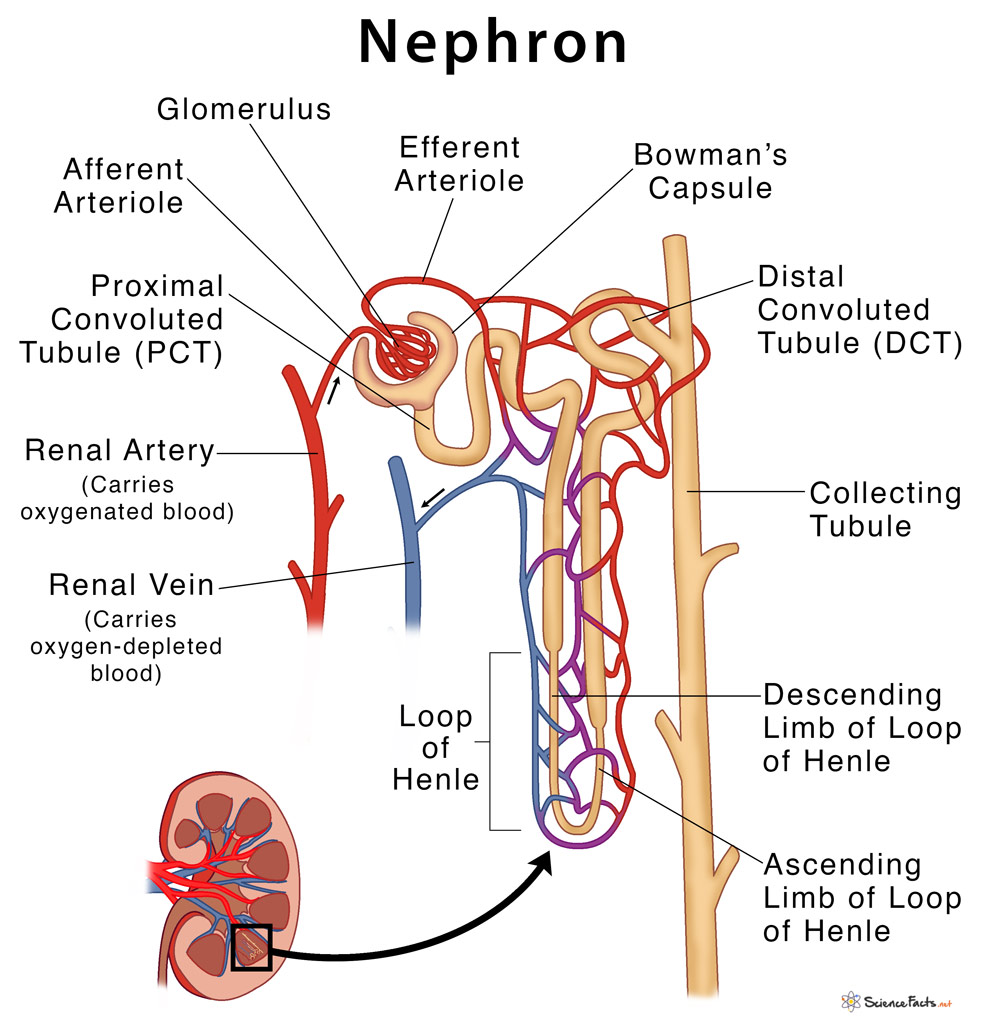
Anatomy of the Nephron
Understanding the nephron’s anatomy is crucial to comprehending how urine is formed. Each nephron consists of two components:
- Renal Corpuscle
- Renal Tubule
Renal Corpuscle
The Bowman’s capsule and the glomerular capillaries, also known as the glomerulus, make up the renal corpuscle. Blood is filtered under high pressure in the renal corpuscle. The afferent arteriole is the artery that supplies blood to the glomerulus, whereas the efferent arteriole is the artery that removes blood from the glomerulus. A network of capillaries known as the glomerular capillaries of the glomerulus develops between these arterioles. This glomerulus is situated in a cup-shaped structure called the Bowman’s capsule. The Bowman’s capsule and glomerulus work together to filter blood to generate urine.
Renal Tubule
The renal tubule is made up with;
- The proximal convoluted Tubule(PCT)
- The U-shaped Loop Of Henle
- The Distal Convoluted Tubule(DCT)
The fluid produced after the blood has been filtered in the renal corpuscle is known as glomerular filtrate. Now, this glomerular filtrate enters the PCT. In contrast to the PCT, which adds urea, creatinine, and uric acid to the filtrate, the PCT reabsorbs chemicals like NaCl, K+, water, glucose, and bicarbonate into the filtrate.
The filtrate leaves the PCT and enters the U-shaped Loop of Henle, where water and other metabolites are reabsorb and secreted. The DCT then receives the filtrate. The filtrate exits the DCT and travels via the collecting tubules, renal pelvis, and ureters to become urine, which is then deposited in the bladder.
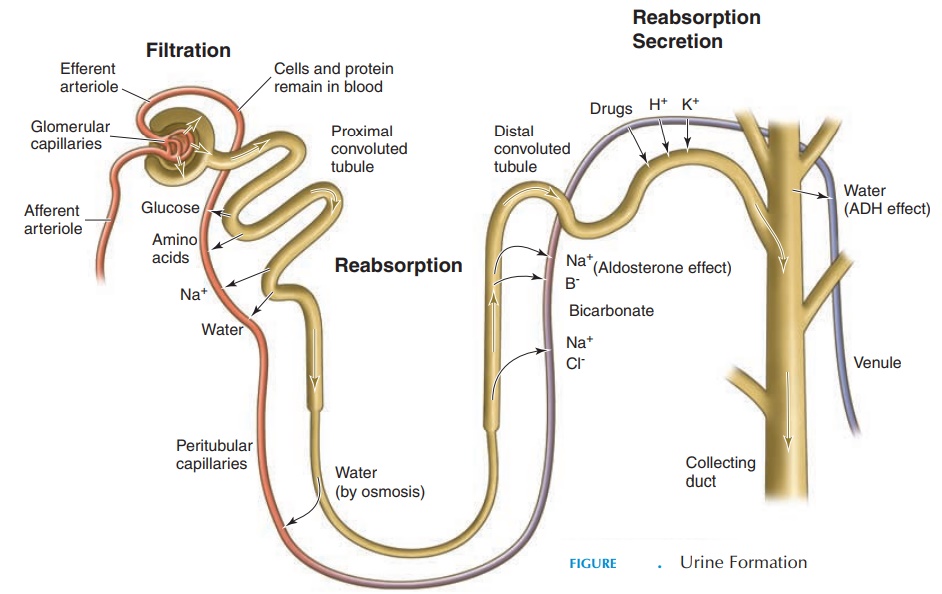
Formation Process
There are three stages to the formation process:
- Glomerular Filtration
- Tubular Reabsorption
- Tubular Secretion
Glomerular Filtration
The glomerular capillaries facilitate this process. An ultrafiltrate develops as a result of the filtration process. High pressure blood rushes into these capillaries and filters through their thin capillary walls. The ultrafiltrate is forced into the capsular area of the Bowman’s capsule, leaving out the blood cells and proteins. The glomerular filtration rate (GFR) is 125 milliliters per minute, or 180 liters per day.
Tubular Reabsorption
All substances—aside from blood cells and proteins—are forced through the capillaries by high pressure during glomerular filtration. Some of the constituents of the filtrate are reabsorbed at the level of the Proximal Convoluted Tubule (PCT). These substances include potassium, glucose, amino acids, sodium chloride, bicarbonate, and 75% water.
Some compounds are passively absorbed, while others are actively transported and still others are co-transported. The permeability of various nephron components affects absorption. Selective absorption is visible in the distal convoluted tubule. The peritubular capillaries absorb the chemicals and water that are reabsorbed to transfer them back to the circulation.
Tubular Secretion
The peritubular capillaries assist in actively secreting molecules like H+ ions and K+ ions in addition to delivering the reabsorbed substances into the bloodstream. In order to keep the Na-K balance, Na+ ions are actively reabsorbed whenever too much K+ is secreted into the filtrate. Some medications are actively secreted into the filtrate during the tubular secretion phase because they are not filtered in the glomerulus.
Composition of Urine
Physical characteristics: The kidneys remove waste products through urine. Waste materials such as urea, salts, extra ions, water, and drug metabolites are all found in urine. The color of fresh urine is often light or pale yellow, and it has a faint ammoniac smell. Often, it has a pH of 4–8, is transparent, and is turbid. The type of sickness present in the body affects these features differently. An analysis of a urine sample is frequently used to find disorders like diabetes, kidney failures, etc.
Chemical composition: Urine contains urea, sodium chloride, potassium ions, creatinine, ammonia products, a little amount of protein, and other metabolites in the majority.
Certain abnormalities in the urine composition
Some of the following conditions result in anomalies in urine composition:
- Hematuria: Hematuria is the medical term for when blood is detected in the urine. This is a pathology sign, possibly associated to an infection or an injury.
- Proteinuria: This is a condition when there are protein molecules in the urine. This suggests that the kidney’s filtration system has a flaw.
- Pyuria– When pus cells are seen in the urine, a condition known as pyuria is present. This suggests that the body may already be infected.
- Glycosuria– This is a condition characterized by the presence of glucose in the urine. This is a sign of diabetes, probably uncontrolled diabetes.