Most pathogenic microbes can develop resistance to some antimicrobial agents, which is known as antimicrobial resistance. It occurs when fungi, bacteria, viruses, and other disease-causing organisms evolve and lose their ability to respond to treatments used to treat them, making diseases more difficult to treat and raising the risk of disease spread and death.
Antimicrobial resistance has emerged as a new cause of death around the world. After the discovery of antibiotics, it was considered that the battle against germs was won, until it was discovered that some of the medications used against them were resistant to them.
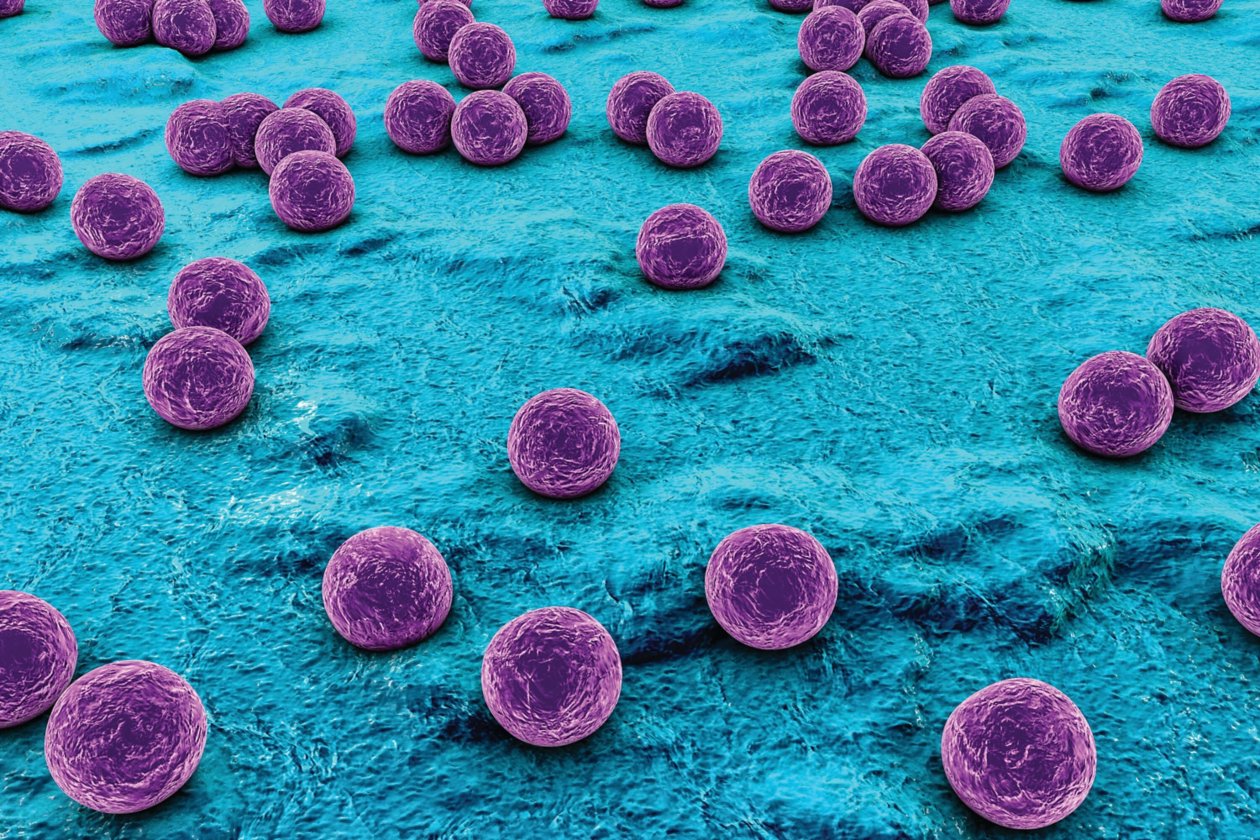
Antimicrobial resistance rises when antibiotics force bacteria and fungi to adapt, resulting in antibiotic-resistant organisms that live and propagate. The more antibiotics a person takes, the greater the potential that bacteria will develop resistance to them. Methicillin-resistant Staphylococcus aureus, Penicillin-resistant Enterococcus, and multidrug-resistant Mycobacterium tuberculosis, which is resistant to both isoniazid and rifampicin, are examples of common bacteria resistant to antibiotics. Formation of biofilms by bacteria has also helped bacteria resist antibiotics.
Antimicrobial resistance mechanisms fall into four major categories;
- Limiting uptake of a drug
- Modifying a drug target
- Inactivating a drug
- Active drug efflux
Understanding these mechanisms leads to improved treatment choices for infectious disorders and the development of antimicrobial medications that are effective against bacteria.
Limiting Drug Take
The structure and functions of the lipopolysaccharide layer in gram negative bacteria operate as a barrier to specific chemicals, allowing some bacteria to become more resistant to antimicrobial drugs. Mycobacteria, for example, have a high-lipid outer membrane, which allows hydrophobic medications to enter the cell more easily than hydrophilic pharmaceuticals, which have limited access.
Bacteria without a cell wall are naturally resistant to all medications that target the cell wall; nevertheless, gram positive bacteria lack an outer membrane and hence are not drug resistant. Staphylococcus aureus, for example, is a gram-positive bacteria that has developed resistance to antimicrobial drug called vancomycin. Staphylococcus aureus produces a thicker cell wall that makes it difficult for the drug to penetrate the cell, resulting in vancomycin resistance.
Drug Target Modification
There are numerous components in bacterial cells that are antimicrobial drug targets, as well as numerous targets that bacteria modify to enable them to resist antimicrobial treatments. Daptomycin, for example, requires the presence of calcium to bind. Gene mutations shift the charge of the cell membrane surface to positive, inhibiting calcium binding, and therefore they resist daptomycin.
Drugs that target nucleic acid synthesis are another example. Modifications in DNA gyrase (gram negative bacteria) or topoisomerase iv cause resistance (gram positive bacteria). These alterations can alter the structure of gyrase and topoisomerase, reducing or eliminating the drug’s capacity to bind to these components.
Inactivating a Drug
This is accomplished in one of two ways: catalytic breakdown of the drug or chemical group transfer to the drug. Tetracycline, for example, is inactivated via hydrolysis through the tetX gene; beta lactamases are a broad category of drug hydrolyzing enzymes. Transfer of a chemical group to the medication is the most prevalent method of inactivation, with acetyl, phosphoryl, and adenyl groups being the most common. The most prevalent method is acetylation, which is used to combat aminoglycosides, chloramphenicol, streptogramins, and fluoroquinolones. The aminoglycosides are predominantly targeted through adenylation and phosphorylation.
Beta lactam medicines are the most extensively used class of antimicrobials, and microbes fight them in three ways:
- Blocking the medicine from interacting with the target PBP.
- The existence of efflux pumps capable of extruding beta lactam medicines.
- Drug hydrolysis by beta lactamase enzymes.
Antimicrobial agents are classified into classes depending on their antimicrobial action mechanism. Inhibitors of cell wall production, depolarizers of the cell membrane, inhibitors of protein synthesis, inhibitors of nucleic acid synthesis, and inhibitors of metabolic pathways in bacteria are the key classes. The following understanding might have helped to properly manage these microorganism, but sadly, poor antimicrobial stewardship has resulted in resistance.
Increased consumption of antimicrobial medications, incorrect prescribing of antimicrobial treatments either by self-medication or clinical misuse, such as prescription of drugs that would prove ineffective for the bacteria causing the sickness, are all factors that have contributed to resistance. Patients who take a lot of antimicrobial medications are more likely to become infected with resistant microorganisms.
Bacteria are not all susceptible to or resistant to the same antimicrobial agents. The minimal inhibitory concentration is used to determine susceptibility and resistance. This is the lowest drug concentration that will stop bacteria from growing. Susceptibility is the range of the average minimum inhibitory concentration for any specific agent across all bacterium species. Bacteria may have inherent antimicrobial resistance or acquire resistance genes from other closely related organisms, resulting in natural and acquired resistance.
Natural resistance can be induced or intrinsic. Intrinsic resistance is always present in the species; it is unrelated to horizontal gene transfer and is independent of previous antibiotic exposure. Genes that are naturally present in bacteria but are only expressed to resistant levels after exposure to antimicrobial drugs are known as induced resistance genes.
Acquired resistance refers to the acquisition of genetic material that provides resistance through the chromosomal DNA transformation, transposition, conjugation, and mutation mechanisms. Permanent or temporary acquired resistance is possible. Transformation, transposition and conjugation are called horizontal gene transfer (HGT).
Ways to Combat Antimicrobial Resistance
Antimicrobial resistance can be reduced in several ways:
- Development of quick diagnostic tests.
- Antibiotics that promote growth should be removed from animal feed.
- New medicines research and development.
- Antimicrobial stewardship should be implemented.
- Collaboration and resource exchange among countries to help fight antimicrobial resistance .
- Antibiotic-resistant bacteria should be monitored more closely.
RELATED: Prevention and Control of Antibiotics Resistance